Pathogens Behind SIBO And Limitations of Rifaximin
Rifaximin, a non-systemic antibiotic, is the standard of care for addressing SIBO [1]. However, it doesn’t work in over 50% of the patients [2]. The fortunate ones get their symptoms reduced but are rarely cured [3]. Further, 64% of the patients who benefit from Rifaximin relapse within a few months [4]. Clearly, a better solution for SIBO is required.
Prior to any serious discussion of potential therapeutic solutions, it is necessary to characterize the small intestinal microbiome and the pathogens behind SIBO. There are relatively few studies that have investigated this because of the technical challenges involved in the intrusive process of extracting duodenal or jejunal aspirate samples. We will highlight the noteworthy ones.
In a recent study, Leite et al [5] identified 42 SIBO & 98 non-SIBO subjects and compared their duodenal aspirates. Here are the two major findings from their paper:
- SIBO patients had 4.3 times higher abundance of Proteobacteria, and 1.64 times lower abundance of Firmicutes – leading to over 7-fold increase in Proteobacteria to Firmicutes ratio for SIBO patients compared to non-SIBO subjects. This has important implications for potential new therapeutics.
- The Increase in Proteobacteria resulted primarily from higher relative abundance from the family Enterobacteriaceae that includes E. coli and Klebsiella pneumoniae.
The study by Pyleris et al [6] with 62 SIBO and 320 total patients pointed towards similar microbial suspects. The most common isolates in SIBO patients were found to be Escherichia coli, Enterococcus spp and Klebsiella pneumoniae. Ghoshal et al [7] analyzed the jejunal aspirate cultures and showed that Escherichia coli, Streptococcus spp, Pseudomonas aeruginosa, Staphylococcus spp, Acinetobacter spp, Enterococcus spp, and Klebsiella pneumoniae were the predominant bacteria found in patients with SIBO.
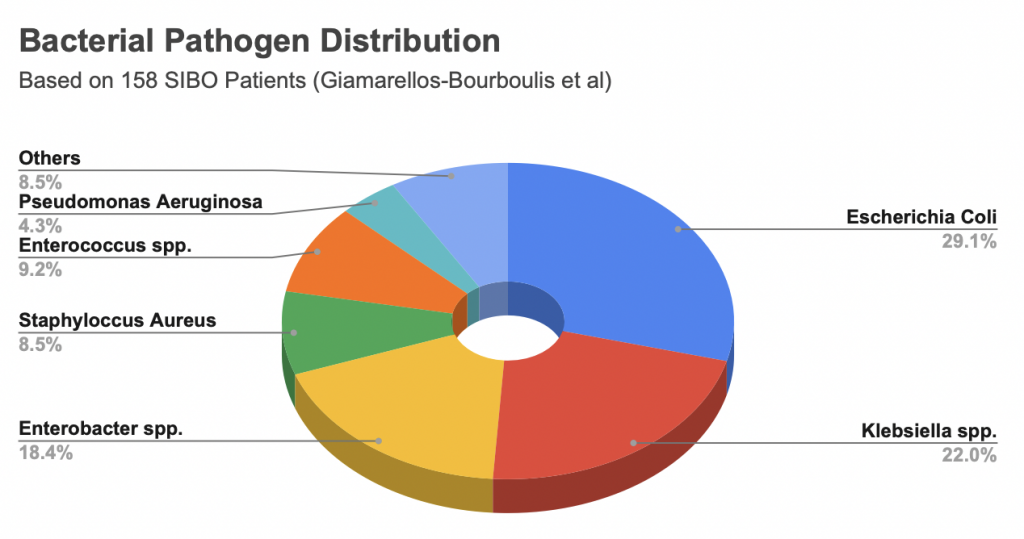
In one of the larger studies, Giamarellos-Bourboulis et al [8] analyzed duodenal aspirate cultures from 897 patients undergoing upper GI endoscopy. 158 of these patients were found to have SIBO. The most common bacterial pathogens based on the duodenal aspirate culture results from these SIBO patients are shown in the Pie Chart above
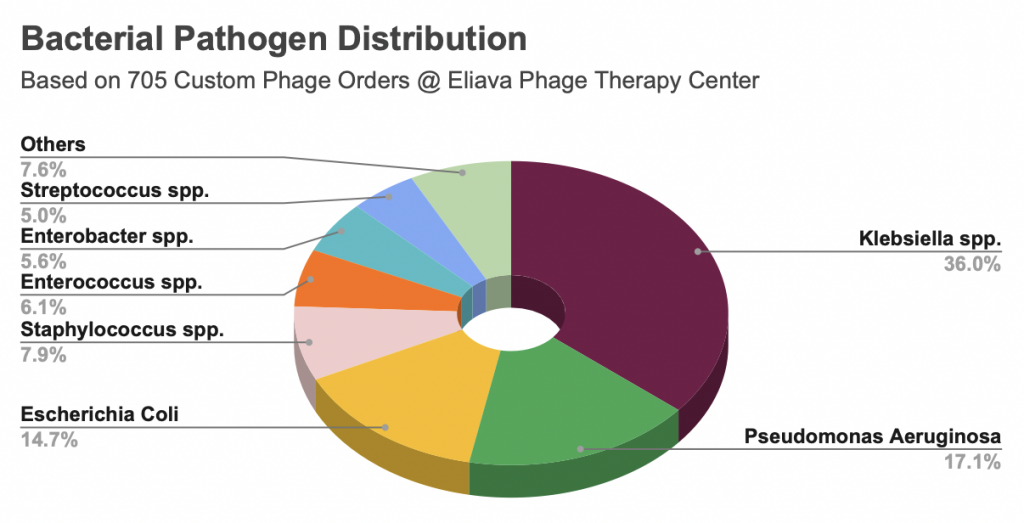
Finally, as a sanity check it is interesting to look at work by Zaldastanishvili et al [9] from Eliava Phage Therapy Center (EPTC). At Eliava, patients with digestive disorders have their stool samples analyzed and treated with Bacteriophages for specific pathogens. While the small intestinal microbiome is markedly different from that in stool as noted by Leite et al [10], the pathogens found in the duodenal aspirates are strikingly similar to the ones found in stool samples by EPTC. The pie chart below provides another perspective in understanding the most common bacterial pathogens in patients with functional gastrointestinal disorders.
In summary, the small intestinal microbiome of SIBO patients is in a state of dysbiosis.
- The proteobacteria to firmicutes ratio in SIBO patients is over 7 times that of a healthy person.
- The most common pathogenic bacteria behind SIBO are E. Coli, Klebsiella, Enterococcus, Staphylococcus, and Enterobacter.
Limitations of Rifaximin
Rifaximin is an excellent broad spectrum antibiotic, which means it will kill all the bacteria – good and bad that come in its way. It does a great job in reducing bacterial overgrowth. However, by design a broad spectrum antibiotic can not improve the Proteobacteria to Firmicutes ratio. In fact, Proteobacteria are primarily gram negative bacteria that are harder to kill than Firmicutes that are primarily gram positive. This implies that use of Rifaximin will at best keep the Proteobacteria to Firmicutes ratio the same, and at worst it will clear the way for a pathogen to take over and colonize even more intestinal space.
A Better Approach
An ideal therapeutic for SIBO can not be a broad spectrum antibiotic, and put the entire microbiome in harm’s way. An ideal therapeutic would only target the pathogens, and create an environment for healthy firmicutes to flourish, thereby restoring the balance between proteobacteria and firmicutes. This is what we are developing at Gutbiotics.
REFERENCES
1. Takakura W, Pimentel M. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome – An Update. Front Psychiatry. 2020 Jul 10;11:664.
2. Shah SC, Day LW, Somsouk M, Sewell JL. Meta-analysis: antibiotic therapy for small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2013;38(8):925–34.
3. Rezaie A, Heimanson Z, McCallum R, Pimentel M. Lactulose Breath Testing as a Predictor of Response to Rifaximin in Patients With Irritable Bowel Syndrome With Diarrhea. Am J Gastroenterol. 2019 Dec;114(12):1886–93.
4. Lembo A, Pimentel M, Rao SS, Schoenfeld P, Cash B, Weinstock LB, et al. Repeat Treatment With Rifaximin Is Safe and Effective in Patients With Diarrhea-Predominant Irritable Bowel Syndrome. Gastroenterology. 2016 Dec 1;151(6):1113–21.
5. Leite G, Morales W, Weitsman S, Celly S, Parodi G, Mathur R, et al. The duodenal microbiome is altered in small intestinal bacterial overgrowth. PLoS ONE. 2020 Jul 9;15(7):e0234906.
6. Pyleris E, Giamarellos-Bourboulis EJ, Tzivras D, Koussoulas V, Barbatzas C, Pimentel M. The Prevalence of Overgrowth by Aerobic Bacteria in the Small Intestine by Small Bowel Culture: Relationship with Irritable Bowel Syndrome. Dig Dis Sci. 2012 May 1;57(5):1321–9.
7. Ghoshal UC, Srivastava D, Ghoshal U, Misra A. Breath tests in the diagnosis of small intestinal bacterial overgrowth in patients with irritable bowel syndrome in comparison with quantitative upper gut aspirate culture. Eur J Gastroenterol Hepatol. 2014 Jul;26(7):753–60.
8. Giamarellos-Bourboulis EJ, Pyleris E, Barbatzas C, Pistiki A, Pimentel M. Small intestinal bacterial overgrowth is associated with irritable bowel syndrome and is independent of proton pump inhibitor usage. BMC Gastroenterol. 2016 Jul 11;16(1):67.
9. Zaldastanishvili E, Leshkasheli L, Dadiani M, Nadareishvili L, Askilashvili L, Kvatadze N, et al. Phage Therapy Experience at the Eliava Phage Therapy Center: Three Cases of Bacterial Persistence. Viruses. 2021 Sep 23;13(10):1901.
10. Leite GGS, Weitsman S, Parodi G, Celly S, Sedighi R, Sanchez M, et al. Mapping the Segmental Microbiomes in the Human Small Bowel in Comparison with Stool: A REIMAGINE Study. Dig Dis Sci. 2020 Sep 1;65(9):2595–604.